How will I be tested for hep C?
The only way to know if you have hepatitis C is to get tested. This involves two simple blood tests.
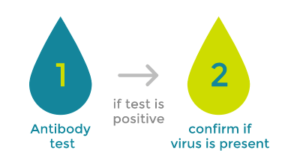
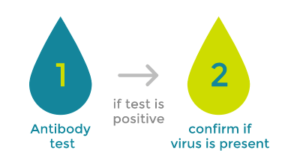
The first will show if you have hep C antibodies. If this test is positive, it means that you’ve been exposed to the hep C virus sometime in your life, either within the past few months or many years ago.
To confirm if you have a current infection, a second test checks for the hepatitis C virus in your blood. It’s very important to have this second test if you test positive for hep C antibodies.
If these blood tests confirm a current infection, your healthcare professional will send you for another blood test or a simple and painless liver scan (also called a FibroScan®) which will give information about the health of your liver. Then, you and your healthcare professional can discuss the results and treatment options.
Getting diagnosed early can prevent liver and health problems that may be caused by the virus as well as keeping it from spreading to someone else by blood contact.
Hep C can be treated
A new hep C infection does not always require treatment and some people can clear the infection within the first 6 months. If the new infection persists beyond this point, it is considered chronic and requires treatment.
With treatment, hep C can be cured*.
A healthcare professional will be able to advise if treatment is required.
*Cure means that the hep C virus is not found in the blood 3 months after the end of treatment.
Hep C risk factors and symptoms
Hepatitis C Checklist
Are you at risk of hep C? It is estimated that thousands of people* in New Zealand are living with hepatitis C but have not yet been diagnosed.
*In 2023 it is estimated that approximately 30,000 Kiwis are living with chronic hep C.
Hep C risk factors
The hep C virus is spread when infected blood (even microscopic amounts) enters your blood stream. The virus can live outside the body for several days to weeks. Because there are a number of ways people can get hep C, this checklist covers many of the risk factors.
You may be at risk of hepatitis C if you can say ‘Yes’ to any of the following:
-
×
Did you know...
Needles puncture your skin when you’re getting a tattoo or piercing which can cause bleeding. If even small amounts of infected blood remain on the tattoo needle or in the ink and the needles and equipment are re-used or not sterilised properly, the virus could be transferred to you during the tattooing process. -
×
Did you know...
Blood was not tested for hep C before 1992 so you may be at risk if you had a blood transfusion before this time. -
×
Did you know...
Sharing or reusing needles and syringes increases the chance of spreading hep C. Syringes with detachable needles increase this risk even more because they can retain more blood after they are used than syringes with fixed-needles. -
×
Did you know...
Hep C is a virus spread by blood-to-blood contact. An injury or illness that requires medical or dental treatment (e.g. injection, IV drip, transfusion) could result in hep C infection if the blood supply is not properly screened and/or the equipment is not disinfected or sanitized. -
×
Did you know...
The overall rate of mother to child transmission of hep C virus infection is 4-10%. -
×
Did you know...
If you've shared needles, syringes, drug equipment or tattooing or piercing equipment while in prison you could be at risk of hep C.
Less common risks include:
-
×
Did you know...
Sexual transmission of hep C is possible. A person's risk for hep C appears to increase if they have a sexually transmitted disease or HIV, sex with multiple partners, or rough sex. -
×
Did you know...
You can get hep C if your blood comes into contact with blood from someone infected with the hep C virus. Only small amounts of blood are needed to spread the virus.
What are the signs of hep C?
Most people with the hepatitis C virus don’t show any symptoms, yet hep C can lead to serious health complications.
In people who do develop symptoms from acute infection, the average time from exposure to symptoms ranges from two to 12 weeks after becoming infected, while others will experience them six months later. In some cases, people can live with hep C for years before they experience any symptoms at all.. Even without symptoms, a person with hep C can still spread the virus to others.
If you’re at risk for hep C, and have experienced any of the symptoms listed below, speak with your healthcare professional and ask if you should be tested.
Symptoms of acute (new) and chronic (long-lasting) hepatitis C infection may include:
-
×
Did you know...
It's common for people living with hep C to feel extremely tired or have no energy. -
×
Did you know...
Loss of appetite can have many causes. If you have a risk factor and frequent loss of appetite talk to your healthcare professional. -
×
Did you know...
Stomach pain can have many causes. If you have a risk factor and stomach pain talk to your healthcare professional. -
×
Did you know...
Nausea can have many causes. If you have a risk factor and frequent nausea talk to your healthcare professional. -
×
Did you know...
Joint pain can have many causes. If you have a risk factor and frequent joint pain talk to your healthcare professional. -
×
Did you know...
Jaundice can appear soon after you're infected with the hep C virus. Your skin and the whites of your eyes may look yellowish. This happens when your liver doesn't work well enough to break down a chemical called bilirubin. Your skin can turn yellow if too much of it builds up in your blood.
Talking to your healthcare professional about hepatitis C
Here are some questions that may help you organise your thoughts when you visit:
- Where do I have to go to be tested?
- What tests do I need?
- What could the results mean?
- Do I need to get tested for hep A and hep B?
Getting tested is the only way to know for sure if you have hep C.
You might find it helpful to download or print this checklist and take it with you to talk to your healthcare professional about your results.
This checklist is not meant to diagnose people with hep C, nor does it replace the advice of your healthcare professional. Please talk to your healthcare professional if you have any questions about hep C.

